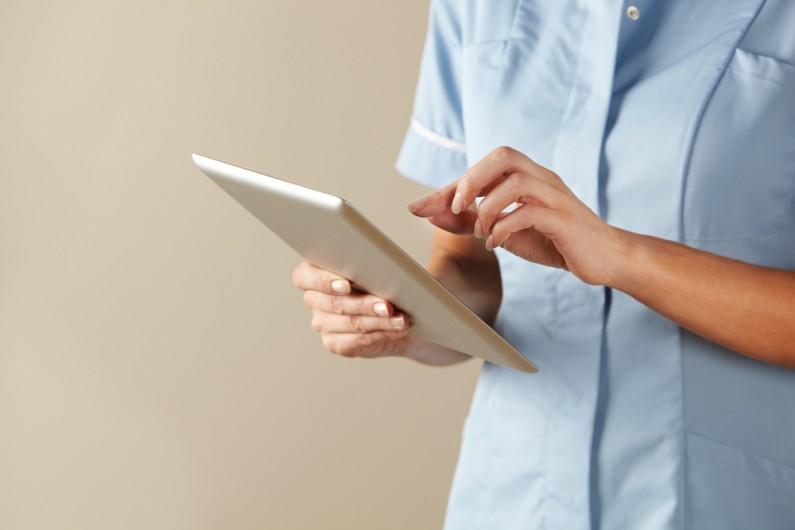
Mobile technology has revolutionised so many aspects of our work and lives. Our home care teams make many visits each day to multiple locations, so mobile technology is the logical way to support the work they do.
The Mobile Care Worker App we recently introduced supports our care teams at all points of service delivery. It means we can forget about completing paper forms and records during visits and focus more time on our care users.
The app guides our staff to each appointment using maps and directions. If there is anything they need to know to gain access, the app will tell them this also.
Once at the appointment, our staff check in automatically using their mobile phone. They can see an up-to-date checklist of the care tasks to be carried out and any other information about the service user that might be relevant. They can also be prompted to check whether medication has been taken and record any details that might help with adapting to the care plan to meet changing care needs.
More Efficient
Mobile Care Worker also helps us organise the care we provide more efficiently. Data is captured instantly from each visit due to staff being able to input information through the app rather than in the office. This means we spend less time entering data from paper forms and more time designing a better service to meet our customers’ needs.
We also spend less time designing visit rosters and can see instantly where all our mobile staff are. If it looks like they might be late for an appointment, we can let people know to reassure them that they haven’t been forgotten. Simpler rostering also makes it easier for us to ensure that people see the same care worker at every visit.
Mobile Care Worker provides another way to involve relatives in the care of their loved one, which can be very welcome if they don’t live locally. They can be given secure access to the system and be reassured that visits have taken place when scheduled. They can also be part of the discussion around designing the most appropriate care programme.
Technology will never take the place of personal interactions in the care delivery, but it can take care of all the things that help those interactions to be more effective.
If you or an elderly relative are starting to find basic household tasks a bit challenging, a care at home service might be just what’s needed to brighten life up. Contact us today on 01305 300161 to find out more or click here.